For decades, healthcare has been shaped by physical infrastructure, human-centred workflows, and incremental digitalisation. Automation reduced some administrative burden. But these changes never challenged the core operating model of healthcare. Now, that model is breaking.
A new wave of evidence — from real-world regulatory pilots to peer-reviewed clinical research and the strategic moves of frontier AI companies — points to a clear conclusion: healthcare businesses must move beyond using AI as a tool and start becoming AI-native. Not later. Now.
From Support Tool to Decision-Making System
In early 2026, Utah became the first US state to allow an AI system to renew routine prescriptions for chronic conditions autonomously. The system, developed by Doctronic, operates within a regulatory sandbox and performs identity checks, patient interviews, and medical history analysis before issuing refills.
State officials reported that the AI’s decisions aligned with physicians’ judgments in more than 99% of cases. This wasn’t a lab experiment. It wasn’t a proof-of-concept prototype. It was a live healthcare decision-making system operating under regulatory oversight.
The significance of this moment goes beyond prescriptions. It marks a shift in how regulators, providers, and patients are beginning to perceive AI: not as a back-office assistant, but as a trusted participant in clinical workflows.
At the same time, peer-reviewed research published in Nature Medicine shows AI systems outperforming traditional methods in predicting disease risk from complex, longitudinal datasets — including sleep patterns and behavioural signals — long before symptoms appear.
Together, these signals point to a deeper change: AI is moving from efficiency support to clinical and strategic relevance.
The Limits of “AI-Enabled” Healthcare
Most healthcare organisations today would describe themselves as “AI-enabled”. They use AI to:
- transcribe consultations,
- automate documentation,
- optimise scheduling,
- assist customer support,
- or analyse population-level data retrospectively.
These improvements matter — but they don’t change the system. AI-enabled healthcare still relies on:
- fragmented data,
- siloed decision-making,
- human bottlenecks,
- and linear care pathways.
In contrast, AI-native healthcare redesigns the system around intelligence from the start.
What Does “AI-Native” Actually Mean in Healthcare?
At The Gradient, we use AI-native to describe businesses that are built on three core principles:
- AI is embedded into the product logic, not added later as a feature
- Decision-making is augmented or led by AI, not just supported
- The user experience is designed around trust, transparency, and automation, not manual intervention
This distinction matters — because it shapes everything from business models to compliance strategies. AI-native healthcare businesses don’t ask, “Where can we plug in AI?” They ask, “What decisions can be made earlier, faster, or more accurately if intelligence is built into the system?”
Why the Market Is Forcing This Shift
The healthcare AI market is projected to grow at over 38% CAGR throughout the next decade, reaching hundreds of billions in value. But growth alone isn’t the most telling signal. More important is where AI investment is concentrating.
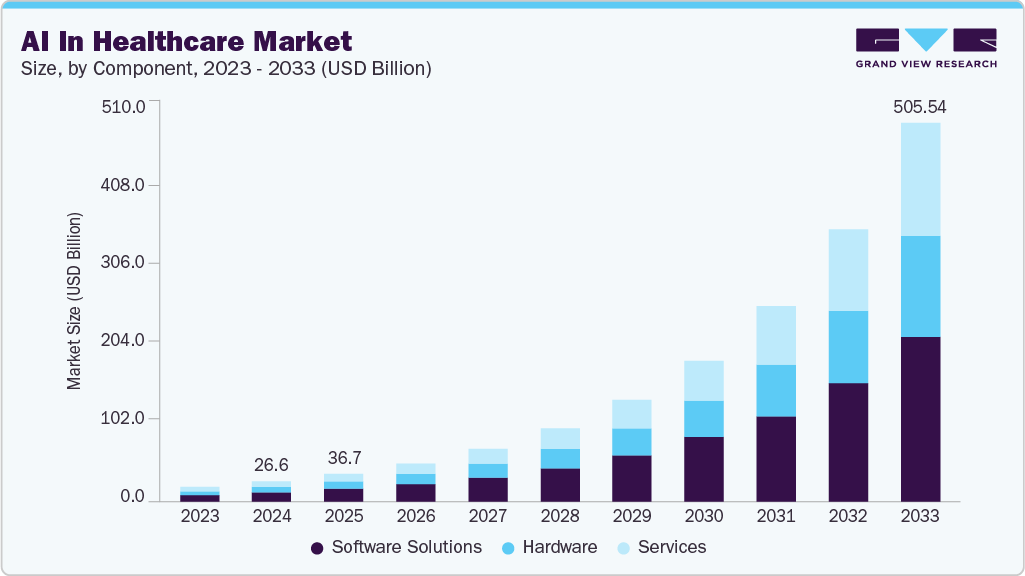
Over 60% of digital health venture funding in 2025 went to AI-driven companies — particularly those focused on predictive care, autonomous workflows, and decision intelligence rather than surface-level automation.
Investors aren’t backing AI because it’s fashionable. They’re backing it because AI-native healthcare scales differently:
- fewer marginal costs,
- fewer human bottlenecks,
- more consistent outcomes across populations.
Frontier AI Companies Are Building Healthcare Infrastructure — Not Experiments
This shift isn’t driven by startups alone.
In 2026, Anthropic announced an expanded healthcare and life sciences strategy, including Claude for Healthcare — a HIPAA-aligned AI system designed to operate inside regulated clinical, insurance, and research workflows.
What’s notable isn’t just compliance. Anthropic is actively integrating AI with:
- medical coding standards (ICD-10),
- clinical trial databases,
- biomedical research repositories,
- and regulatory documentation processes.
In other words, frontier AI companies are no longer experimenting at the edges of healthcare. They are building core infrastructure that healthcare organisations will either adopt or compete against.
This is a critical signal for healthcare leaders: AI capability is becoming a foundational layer of the ecosystem, not an optional enhancement.
Alongside infrastructure-level moves by companies like Anthropic, the launch of ChatGPT Health by OpenAI signals a parallel shift on the consumer side. AI is increasingly becoming the first point of contact for health-related questions — helping people reason about symptoms, risks, and next steps before they ever enter a clinical system.
Google is pushing this shift even deeper into clinical reality. With the release of MedGemma 1.5, Google introduced a multimodal foundation model designed for medical image interpretation — capable of analysing X-rays, CT scans, and structured medical records together. Alongside it, MedASR extends AI directly into clinical workflows by accurately transcribing medical speech and terminology in real time, reducing the need for manual documentation during diagnostic and imaging procedures.
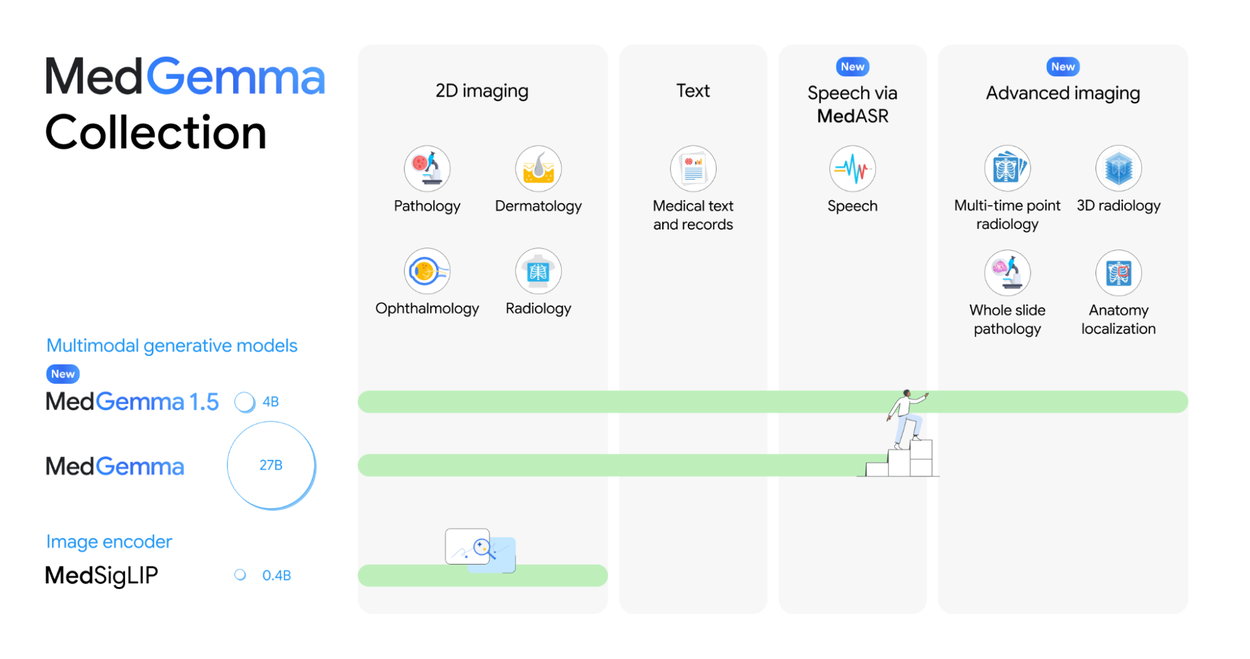
Taken together, these efforts point to the same conclusion: frontier AI companies are no longer experimenting at the edges of healthcare. They are building foundational layers of medical intelligence — models and systems that healthcare businesses will need to integrate, rather than replicate. AI capability is becoming a core part of the healthcare stack, not an optional enhancement.
From Efficiency Gains to Systemic Clinical Value
The first wave of healthcare AI focused on operational relief. The next wave is about clinical and strategic value at scale.
AI-native systems can:
- identify high-risk patients before deterioration,
- personalise care pathways continuously,
- reduce unnecessary appointments and interventions,
- allocate clinical resources dynamically,
- and support preventative rather than reactive care.
This is not about replacing clinicians. It’s about redesigning healthcare systems, so clinicians spend their expertise where it matters most — while intelligence operates continuously in the background.
AMS Health: What an AI-Native Healthcare Product Looks Like in Practice
Our work on AMS Health shows what it means to design an AI-native healthcare product for real clinical environments — not speculative futures.
AMS Health is an AI-powered healthcare platform designed to support clinical decision-making and operational workflows across complex care settings. The product focuses on one of healthcare’s most persistent problems: fragmented data, delayed insights, and reactive decision-making.
Instead of layering AI on top of existing systems, AMS Health was designed around intelligence from the start.
The platform brings together:
- structured clinical data,
- patient history and ongoing signals,
- and AI-driven analysis that continuously interprets this information in context.
Rather than acting as a static reporting tool, AMS Health is built to:
- surface clinically relevant signals earlier,
- highlight emerging risks and anomalies,
- support prioritisation and decision-making in time-sensitive situations,
- and reduce cognitive and operational load on healthcare teams.
AI is not positioned as an assistant on the side. It is embedded into how the system thinks, surfaces information, and guides action — shaping workflows rather than merely accelerating them.
This is the core difference between AI-enabled and AI-native healthcare. AMS Health doesn’t digitise existing clinical processes or replicate legacy dashboards with smarter analytics. It reimagines how healthcare systems can operate when intelligence is always on — continuously analysing, learning, and supporting decisions at scale.
Regulation Is No Longer a Blocker — It’s a Catalyst
One of the most persistent myths in healthcare is that regulation slows innovation. In reality, regulation is evolving.
Regulatory sandboxes — like Utah’s AI prescription pilot — allow controlled, real-world testing of autonomous systems under strict oversight. Rather than blocking progress, they create frameworks for responsible deployment.
Healthcare businesses that engage early with regulators, design for explainability, and build trust mechanisms into their products are gaining a strategic advantage — not friction.
The Strategic Question Healthcare Leaders Must Answer
The most important question facing healthcare organisations today isn’t: “Should we use AI?” It’s this: “Are we building a healthcare business that can operate when intelligence becomes the default?” Because that future is arriving faster than most legacy systems can adapt.
AI-native healthcare businesses will:
- move faster,
- scale more predictably,
- deliver better outcomes,
- and redefine patient expectations.
Those that treat AI as an add-on will struggle to keep up — not because their technology is worse, but because their operating model is outdated.
Conclusion: AI-Native Is No Longer Optional
Healthcare is shifting from a labour-intensive industry to a decision-intelligent ecosystem.
AI-native businesses aren’t just more efficient — they are structurally different. They are designed for prediction, prevention, and scale.
The organisations that embrace this now will shape the next era of healthcare. The rest will be forced to follow — or fade into irrelevance.